Why This Matters:
Periodontal risk assessment helps us predict disease, intervene earlier, and lower the total burden of inflammatory illness. The latest review underscores a practical, chairside approach that links oral findings with systemic risks – and makes referral timing clearer.

Key Takeaways for Your Practice:
- Risk is multidimensional.Periodontal status reflects modifiable habits (e.g., tobacco, vaping), systemic disease control (diabetes, CVD, CKD) and life stage (pregnancy, aging).
- Bidirectional links are real.Periodontitis can worsen glycemic control and may influence cardiovascular, respiratory, renal and neuroinflammatory conditions.
- Early, targeted intervention wins.Brief chairside risk screens and tailored hygiene/behavioral counseling improve healing and can reduce downstream costs.
- Team sport.Periodontal findings warrant communication with PCPs/endocrinology/cardiology when risks cluster (e.g., elevated BP, high HbA1c, anticoagulation).
- Former smokers ≈ nonsmokers.Smoking cessation meaningfully improves periodontal and implant outcomes.
Quick Risk Snapshot (use at recall or NP exam):
Modifiable
| Systemic / life-stage
|
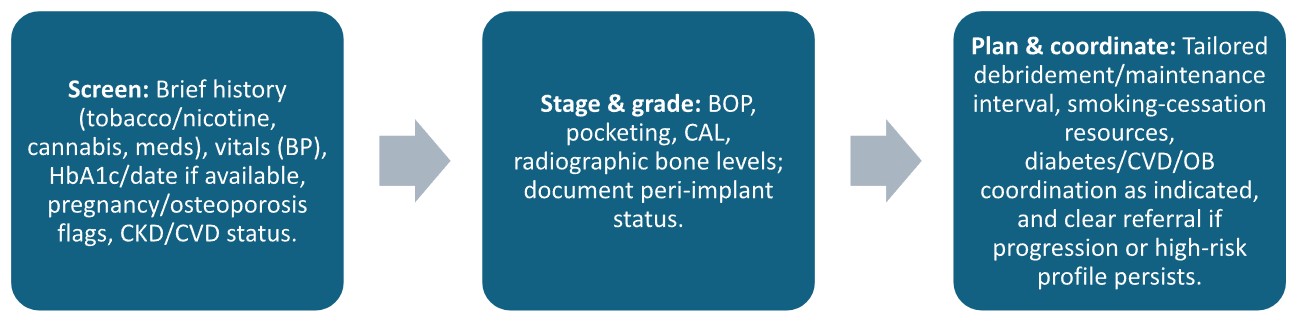
A 3-Step Chairside Workflow:
When to Refer Promptly:
- Non-responsive inflammation after appropriate SRP and 3–4-mo maintenance
- Rapid attachment/bone loss, deep pockets, furcations or peri-implantitis
- Poor wound healing in the setting of tobacco/cannabis/vaping, uncontrolled diabetes, CKD, antithrombotics or pregnancy
- Suspected medication-induced gingival enlargement or anti-resorptive concerns pre-surgery
Practical Counseling Cues You Can Copy/Paste
- Diabetes:“Your gum inflammation can make glucose harder to control; let’s coordinate with your PCP and tighten your periodontal maintenance.”
- Nicotine/Cannabis/Vaping:“These products shift the oral microbiome and slow healing; quitting markedly improves treatment outcomes.”
- Pregnancy:“Treating gum inflammation during pregnancy is safe and may lower adverse outcomes; we’ll increase home care and maintenance.”
- CVD/Antithrombotics:“We’ll use local hemostatic measures and, if needed, consult your cardiology team before surgery.”
Source: Warren, Roger N., D.D.S.; Umbrio, Liana, D.D.S.; and Palomo, Leena, D.D.S., M.S.D. (2025). Practicing Dentistry in the Age of Periodontal Risk Management.The New York State Dental Journal, 91(4), Article 6. Available at: https://commons.ada.org/nysdj/vol91/iss4/6
Comments are closed.